To date, the numerous osteoinductive potential of bonemorphogeneticprotein 2 (BMP-2) non-viral gene remedy can’t be totally exploited therapeutically. This is especially on account of weak gene supply and transient expression peaks limiting the therapeutic impact.Our goal was to check the applying of minicircle DNA, permitting extended expression potential.
It affords notable benefits over typical plasmid DNA. The lack of bacterial sequences and the ensuing discount in dimension, allows protected utilization and improved efficiency for tissue regeneration.We inserted an optimized BMP-2 gene cassette with minicircle plasmid know-how. BMP-2 minicircle plasmids have been produced in E. coli yielding plasmids missing bacterial againbone components. Comparative research of these BMP-2 minicircles and typical BMP-2 plasmids have been carried out in vitro in cell methods, together with bone marrow derived stem cells.
Tests carried out included gene expression profiles and cell differentiation assays.A C2C12 cell line transfected with the BMP-2-Advanced minicircle confirmed considerably elevated expression of osteocalcin, alkaline phosphatase (ALP) exercise, and BMP-2 protein quantity when in comparison with cells transfected with typical BMP-2-Advanced plasmid. Furthermore, the plasmids present suitability for stem cell approaches by exhibiting considerably greater ranges of ALP exercise and mineralization when launched into human bone marrow stem cells (BMSCs).We have designed a extremely bioactive BMP-2 minicircle plasmid with the potential to fulfil medical necessities for non-viral gene remedy within the discipline of bone regeneration.
BMP and TGFß Use and Release in Bone Regeneration
A fracture that doesn’t unite in 9 months is outlined as non-union. Non-union is widespread in fragmented fractures and massive bone defects the place vascularization is impaired. The distal third of the tibia, the scaphoid bone or the talus fractures are moreover susceptible to non-union. Open fractures and spinal fusion instances additionally want particular monitoring for therapeutic.
Bone tissue regeneration could be attained by autografts, allografts, xenografts and artificial supplies, nevertheless their restricted availability and the elevated surgical time in addition to the donor web site morbidity of autograft use, and decrease chance of success, elevated prices and illness transmission and immunological response chance of allografts oblige us to search out higher options and new grafts to beat the cons.
A correct biomaterial for regeneration ought to be osteoinductive, osteoconductive, biocompatible and mechanically appropriate. Cytokine remedy, the place development elements are launched both exogenously or triggered endogenously, is one of the generally used technique in bone tissue engineering.
Transforming development issue ß (TGFß) superfamily, which could be divided structurally into two teams as bone morphogenetic proteins (BMPs), development differentiation elements (GDFs) and TGFß, Activin, Nodal department, Mullerian hormone, are recognized to be produced by osteoblasts and different bone cells and current already in bone matrix abundantly, to take roles in bone homeostasis.
BMP household as the most important subfamily of TGFß superfamily can be reported to be the best development elements in bone and improvement, which makes them one of the preferred cytokines utilized in bone regeneration. Complications relying on the surplus use of development elements, and pleiotropic features of BMPs are nevertheless the primary causes of why they need to be approached with care. In this evaluate, the Smad dependent signaling pathways of TGFß and BMP households and their relations and the purposes in pre-clinical and medical research might be briefly summarized.
The goal of this research was to develop novel hydroxyapatite (HAP)-based bioactive bone substitute supplies for segmental osteotomy reconstruction. Customized three-dimensional (3D) bone assemble was manufactured from nanohydroxyapatite (nHAP) with poly(lactide-co-glycolide) (PLGA) coating utilizing 3D fashions derived from the computed tomography (CT) scanning of the rabbit’s ulna and gradient 3D printing of the bone substitute mimicking the anatomical form of the pure bone defect.
Engineered assemble revealed ample micro-architectural design for profitable bone regeneration having a complete porosity of 64% and a mean pore dimension of 256 μm. Radiography and micro-CT evaluation depicted new bone apposition by means of the entire size of the reconstructed ulna with a small space of non-resorbed assemble within the central space of defect.
Histological evaluation revealed new bone formation with each endochondral and endesmal sort of ossification. Immunohistochemistry evaluation depicted the presence of bone formation indicators – bone morphogenetic protein (BMP), osteocalcin (OCN) and osteopontin (OPN) inside newly fashioned bone. Manufactured personalised assemble acts as a “good” responsive biomaterial succesful of modulating the performance and potential for the personalised bone reconstruction on a clinically related size scale.
KMN-159, a novel EP4 receptor selective agonist, stimulates osteoblastic differentiation in cultured complete rat bone marrow
KMN-159 is the lead compound from a sequence of novel difluorolactam prostanoid EP4 receptor agonists aimed toward inducing native bone formation whereas avoiding the inherent unwanted side effects of systemic EP4 activation. KMN-159 is a potent, selective small molecule possessing pharmacokinetic properties amenable to native administration.
Unfractionated rat bone marrow cells (BMCs) have been handled as soon as at plating with escalating doses of KMN-159 (1 pM to 10 μM). The ensuing elevated alkaline phosphatase (ALP) ranges measured 9 days post-dose are in keeping with elevated osteoblastic differentiation and publicity to KMN-159 at low nanomolar concentrations for as little as 30 minutes was enough to induce full osteoblast differentiation of the BMCs from each sexes and regardless of age.
ALP induction was blocked by an EP4 receptor antagonist however not by EP1 or EP2 receptor antagonists and was not induced by EP2 or EP3 receptor agonists. Addition of BMCs to plates coated with KMN-159 24 days earlier resulted in ALP activation, highlighting the chemical stability of the compound. The expression of phenotype markers comparable to ALP, sort I collagen, and osteocalcin was considerably elevated all through the osteoblastic differentiation timecourse initiated by KMN-159 stimulation.
An elevated quantity of tartrate-resistant acid phosphatase-positive cells was noticed KMN-159 or PGE2 handled BMCs however solely within the presence of exogenous receptor activator of nuclear issue kappa-Β ligand (RANKL). No change within the quantity of adipocytes was noticed. KMN-159 additionally elevated bone therapeutic in a rat calvarial defect mannequin with a therapeutic fee equal to recombinant human bone morphogenetic protein-2.
Our research present that KMN-159 is ready to stimulate osteoblastic differentiation with a really quick time of publicity, supporting its potential as a therapeutic candidate for augmenting bone mass.
Bone-stimulatory therapeutics embrace bone morphogenetic proteins (e.g. BMP2), parathyroid hormone, and antibody-based suppression of WNT antagonists. Inhibition of the epigenetic enzyme Enhancer of Zeste Homolog 2 (EZH2) is each bone-anabolic and osteo-protective.
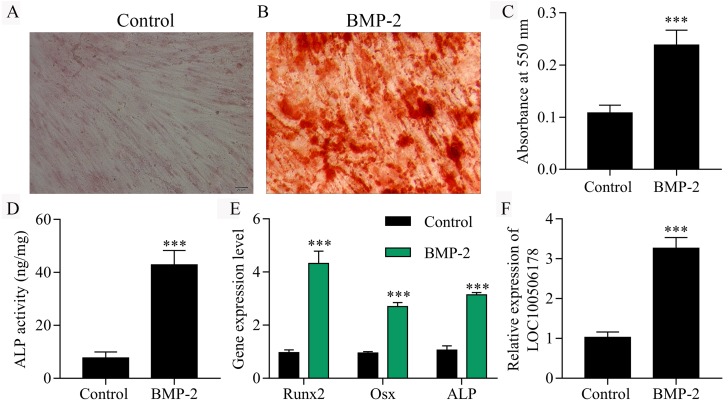
EZH2 inhibition stimulates key elements of bone-stimulatory signaling pathways, together with the BMP2 signaling cascade. Because of excessive prices and opposed results related to BMP2 use, right here we investigated whether or not BMP2 dosing could be diminished by co-treatment with EZH2 inhibitors. Co-administration of BMP2 with the EZH2 inhibitor GSK126 enhanced differentiation of murine (MC3T3) osteoblasts, mirrored by elevated alkaline phosphatase exercise, alizarin crimson staining, and expression of bone-related marker genes (e.g. Bglap and Phospho1).
Strikingly, co-treatment with BMP2 (10 ng/ml) and GSK126 (5 μM) was synergistic and was as efficient as 50 ng/ml BMP2 at inducing MC3T3 osteoblastogenesis. Similarly, the BMP2-GSK126 co-treatment stimulated osteogenic differentiation of human bone marrow-derived mesenchymal stem/stromal cells, mirrored by induction of key osteogenic markers (e.g. Osterix/SP7 and IBSP).
A mixture of BMP2 (300 ng native) and GSK126 (5 μg native and 5 days of 50 mg/kg systemic) yielded extra constant bone therapeutic than single therapies with both compound in a mouse calvarial critical-sized defect mannequin based on outcomes from μCT, histomorphometry, and surgical grading of qualitative X-rays. We conclude that EZH2 inhibition facilitates BMP2-mediated induction of osteogenic differentiation of progenitor cells and maturation of dedicated osteoblasts. We suggest that epigenetic priming, coupled with bone anabolic brokers, enhances osteogenesis and may very well be leveraged in therapeutic methods to enhance bone mass.
